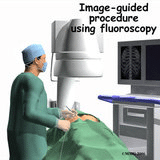
Figure 1
Interventional pain management has come a long way since its humble beginnings several decades ago. What was once a sideline activity for most anesthesiologists has evolved into a highly technical field of medicine. Today, with a large body of peer-reviewed literature documenting the validity and efficacy of interventional pain management techniques, subspecialty training and board certification have become standard. Early on, injections were performed by anesthesiologists using little more than a comprehensive knowledge of anatomy and the occasional plain x-ray. As a result, the practice was more art than science, leading to frustration for both the physician and patient. The advent of fluoroscopically guide injections has transformed the specialty and enabled highly selective diagnostic and therapeutic procedures to be performed safely and with minimal discomfort (see Figure 1).
What follows are some examples showing the positive impact interventional pain management can have on the lives of your patients.
Back in the Game
Jack loves golf. He plays 18 holes two times a week and goes to the driving range when he can to hone his skills. One day, he noticed a mild stab of pain in his lower back after finishing his backswing. As the mild stab became more painful, it interfered with his swing, his score and his enjoyment of the game. He went to his physician and his physical exam, x-rays and even an MRI scan were all normal.
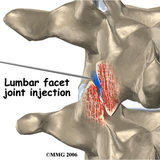
Figure 2
After physical therapy and massage provided only minimal relief, he was referred him for “an epidural”. When I examined Jack, we could recreate his pain by mimicking his golf swing. Under fluoroscopic examination, his tenderness was most pronounced over his right L4-L5 facet joint. He was given a mild sedative and then a small dose of cortisone along with local anesthetic was injected into the facet joint under fluoroscopic guidance (see Figure 2). His pain immediately resolved and he was able to return to his favorite sport. We believe that he had a small tear in the capsule of the facet joint that was too small to be seen on an MRI. The associated pain and inflammation responded to the cortisone injection and the tear healed spontaneously.
Interventional Pain Management: A Mystery Solved
While modern imaging techniques such as MRI and CT scanning are wonderful tools for understanding normal anatomy and abnormalities of the spine, they are of only limited value in determining the actual causes of spine–related pain. For example, on MRI scans, most people older than 40 years of age have some degree of disc degeneration but only rarely is it the cause of back pain. Conversely, many structures that appear normal by imaging studies can indeed be painful. The techniques used by the interventional pain physician are valuable in diagnosing the source of spine-related pain.
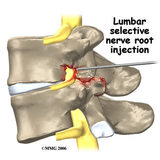
Figure 3
Freddie gradually developed severe pain in his right buttocks that radiated to his lower leg. While his surgeon felt his pain was consistent with irritation of the L5 nerve root, an MRI showed disc bulging at several spinal levels and no apparent involvement of the L5 nerve root. Upon closer inspection, the L5 neuroforamen (the window the nerve uses to exit the spinal canal, see Figure 3) did appear to be narrowed by a small bony projection.
Before recommending surgery, the surgeon felt that he required more evidence that this protrusion was the source of Freddie’s pain. Under fluoroscopic guidance, a small needle was advanced to the L5 nerve root as it exited the neuroforamen. A small amount of x-ray dye was injected in order to outline the nerve root. Importantly, the dye did not spread to any other structures that might also be a source of pain. This was followed by injection of an equally small amount of local anesthetic.
The only discomfort that Freddie felt was a slight amount of pressure and burning in the distribution of his typical leg pain. Within 10 minutes, his leg pain was completely resolved. This result verified the surgeon’s clinical impression that Freddie’s pain was from irritation of the L5 nerve root and that, most likely, the pain was from a narrowed neuroforamen. Freddie subsequently underwent a routine surgical procedure called a foraminotomy and enjoyed complete pain relief.
A Great Help
When patients are not candidates for surgery due to poor health, the severity of symptoms often can be alleviated and the quality of life improved with minimally invasive fluoroscopically guided procedures. Marie’s health had been failing for many years and it had been harder for her to get around. She loved to go on short walks in the neighborhood with her husband but could barely walk one block before experiencing severe burning and aching pain in her back, buttocks and thighs. She had given up her cane and used a walker because she was afraid of falling. A CT scan showed that she had severe spinal stenosis but both her physician and surgeon agreed that her age and poor health precluded an operation. They recommended a conservative approach using physical therapy and fluoroscopically guided injections. After three weeks and two transforaminal epidural injections at the level of the stenosis, she was able to stop using her walker. Her relief will likely not be permanent and she may require more injections in the future, but she is happy to have control over her life again.
Useful Pain Treatment Options with Interventional Pain Management
The examples presented here demonstrate the utility of fluoroscopically guided injections for the treatment of pain in the lumbar spine. These techniques can also used to treat painful conditions of the cervical spine as well as some types of headaches and facial pain. Interventional pain management offers a safe, effective and minimally-invasive approach that is both diagnostic and therapeutic.
