According to the CDC, 43 million Americans have been diagnosed with arthritis. Another 23 million have chronic arthralgia. Arthritis is the leading cause of disability in the United States. It’s no wonder that last year over 600,000 knee replacements were performed in the United States. Total knee arthroplasty (TKA) is a rapidly evolving field of orthopedic surgery. But with any novel technology or technique comes controversy.
INJECTIONS
Each year millions of Americans receive intra-articular knee injections for temporary management of osteoarthritis. Corticosteroids are most commonly used and can offer months of relief in a responsive patient. Intra-articular injection of non-steroidal anti-inflammatories such as Ketoralac have been studied in glenohumeral arthritis with equivalent results to corticosteroids. Theoretically, NSAIDs minimize chondrocyte toxicity, but further studies are necessary to determine the risk/benefit profile of injectable NSAIDs in the knee. Viscosupplementation with injected hyaluronic acid (HA) has gained popularity over the past decade. However, a recent meta-analysis suggests that the clinical benefit from such injections is minimal. The pooled results also suggest that HA may increase the risk of flare-ups and serious adverse events.
MATERIALS

Figure 1
Few innovations in orthopedics have matched the success seen with highly crosslinked polyethylene (XLPE) (see Figure 1). Conventional polyethylene has been used as a bearing surface in hip and knee arthroplasty for decades, but like any plastic it is subject to deformation and wear over time. In 1999, the FDA approved the first generation of XLPE. Irradiating (and thereby crosslinking) polyethylene dramatically improves its wear resistance and durability. Recent data predicts greater than 95% survival of implants at 15 years.
UNICOMPARTMENTAL ARTHROPLASTY
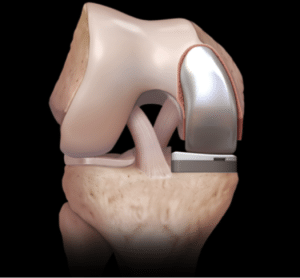
Figure 2
Unicompartmental knee arthroplasty (UKA), or “partial knee replacement” is a procedure growing in popularity with greater than 50,000 performed annually (see Figure 2). This is a good option for patients with arthritis isolated to one area of the knee and without significant deformity or ligament injury. Patients must be selected carefully as the risk of revision is substantially greater than in TKA (usually due to progression of unrecognized arthritis in another area of the knee).
COMPUTERS & ROBOTS

Figure 3
The use of computers and robots in knee replacement has gained significant press in recent years (see Figure 3). In short, computer/robot-assisted knee arthroplasty seems to improve component alignment, but has not been shown to have any effect on clinical outcomes. Furthermore, they increase the operative time and cost of surgery. Such adjuncts are very useful in patients with substantial deformity or retained hardware from prior surgical procedures.
PATIENT SPECIFIC INSTRUMENTS

Figure 4
Patient specific instrumentation (PSI) is a relatively new technology in TKA (see Figure 4). The process involves mapping the patient’s bones with a pre-operative CT or MRI, then customizing guides (not the implants) to assist the surgeon intra-operatively. Like computers, PSI has the potential to improve accuracy of component position, albeit with the added cost of additional pre-operative imaging and the manufacture of custom instruments. PSI can also be very useful in patients with substantial deformity or retained hardware from prior surgical procedures.
VOLUME
Most total knees are implanted by “general” orthopedists with a volume of <30 such cases annually. Recent outcomes data has reaffirmed that surgeons who perform >50-100 knee replacements/year have significantly improved outcomes, including decreased revision rates, infection and length of hospital stay. Patients should be encouraged to seek care from an orthopedist fellowship trained in joint replacement.
